AUGMENTATION MAMMOPLASTY
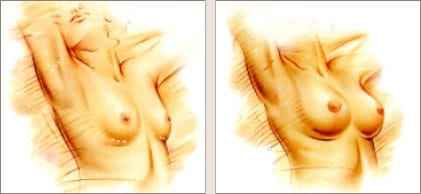
THE GOAL: to enlarge or reshape the breasts and enhance cleavage to those unhappy with small breasts or those whose breasts have lost volume due to aging, pregnancy, nursing or changes in weight.
Breast Augmentation Terminology Notes
- Silicone implants filled with a safe FDA-approved medical-grade silicone gel that achieves the most natural-feeling results
- Saline implants filled with a safe viscous salt-water solution
Dr. Haworth will choose an appropriate incision site so that scars will fade to nearly invisible.
Candidates for Augmentation
The most appropriate candidates for augmentation mammoplasty are:
- A woman who wishes to have larger breasts and WITH a more pronounced cleavage and more appealing shape
- A patient wanting to replace lost volume (especially in the upper pole of the breast) after pregnancy, nursing or notable weight loss
- A patient needing to balance a difference in breast size (either from congenital problems such as Poland’s syndrome or minor natural asymmetries)
- A patient requiring reconstruction following breast cancer surgery
What breast augmentation cannot do is:
- Lift existing sagging breasts more that a breast lift can. It can rotate nipples that point slightly downwards up to a small degree.
- Prevent sagging over time due to gravity, weight gain or unprotected sun exposure
OLD THINKING VS. NEW TECHNIQUES
Breast augmentation has become significantly more sophisticated than in generations past, resulting in a far more natural outcome than ever before.
These breakthroughs include:
- No-Touch Technique: By minimizing contact with the actual breast tissue when the surgeon is inserting the implant into created pocket, bacterial contamination is avoided as well as the risk of capsular contraction.
- More Natural Muscle Draping: Placing the implant under the muscle eliminates the telltale signs and ‘frisbee rim’ sign of implants. Dr Haworth can manipulate the pectoralis muscle in different ways when placing the implants “under the muscle” to maximize a natural look individually for each patient.
- Pocket Placement: The art of pocket making is real proof of a surgeon’s skill. It is vitally important that all dimensions of the pocket are controlled within millimeters to maximally ensure good cleavage, perfect symmetry, beautiful shape and proper implant placement.
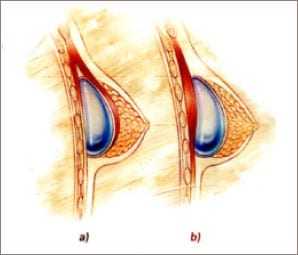
A. Underneath the pectoral is muscle, offering the advantage of looking more natural with less sag, healing with less capsular contraction and making future mammograms easier to read. However, this site may also be more uncomfortable during recovery and require a bit more healing time. However, discomfort is dramatically lessened by approximately 85% because Dr. Haworth instills a long-acting local anesthetic into the breast pocket before closing the incision.
B. Directly behind existing breast tissue but above the muscle. Dr. Haworth rarely uses this technique due to the aforecited reasons.
The 4 options for incision sites are:
1. Under the breast (inframammary) where the crease meets the wall. No scar ever disappears entirely and this one is no exception. It often gets darker (hyperpigments) and is located in potentially quite a visible area especially with the arms outstretched while lying on a beach. I will use this approach if a scar already exists in this location or if other approaches are imprudent.


2. Around the nipple’s areola. This happens to be the most versatile of incisions since it offers the surgeon the most visibility and therefore control during the surgery while healing to a near invisible scar in the majority of patients.
Besides, this is a hidden scar, only visible to your partner or pet! All other scar locations are public ones, possibly leading to embarrassing excuses.


3. In the arm pit (axilla). Again, this often hyperpigments (especially in olive-skinned patients) and results in a higher frequency of misplaced implants and asymmetry.
4. In the navel (umbilicus). This results often in implant malposition. This is not available with silicone gel implants.

Pre-Operative Consultation
The pre-operative consultation is where you meet with Dr. Haworth and our staff to review your health, work out the details of your procedures, order appropriate tests, prescribe medications, discuss your aftercare and answer any questions you may have.
All patients are required to be medically-cleared along with routine blood tests before surgery. For those over 35 or those younger with a family history of breast cancer an up to date mammogram is required. For patients over 45, we may also require a recent chest X-Ray and EKG. We can arrange this for you or, alternatively, you may ask your private English-speaking medical doctor to assist you with this requirement. Our office will facilitate you along the way.
To the consultation, we ask if you could bring photos of your breasts when you were younger and/or before bearing children, and Photos of breasts you like and don’t (Playboy magazine and the internet can be a good place for source material).
CRITICAL PRE-OP CAUTIONARY NOTE
It is absolutely essential that that you avoid all aspirin, aspirin-related, ibuprofen or blood-thinning medications for 2 full weeks prior to your surgery. In your pre-op consultation, we will give you a complete list of these drugs. For our patients, we also provide a password-protected link allowing you to download the list onto your computer. If in doubt about a specific medication, do not take it, call the office first and ask if it is on the forbidden list
Operation and Recovery Logistics
SURGERY DURATION: 1 to 2 hours
ANESTHESIA: General.
Dr. Haworth places a long-acting numbing agent within the breast pocket to minimize any post operative pain in your breast.
As you wake up from surgery, you’re likely to feel tired and slightly sore (particularly in the back). However, we will give you prescription painkillers which will easily control the discomfort.
There will be tape for support over the sutured incision sites and gauze dressings over your breasts. The day after surgery, we will remove the dressings and may provide you an appropriate bra that you should wear continuously for 4 to 12 weeks. Rarely do sutures need to be removed since Dr Haworth employs specific closure techniques with absorbable sutures.
Post-Operative Care
In person and in your post-op information packet, we shall explain everything you need to know for your aftercare at home.
RECOVERY
You will need to keep your activities to a minimum for at least 3 to 5 days. Gradually, you will be able to resume to your normal activities:
- 2-3 DAYS – long walks, no impact
- 3 WEEKS – gentle no-impact exercise (NO Pilates, NO Yoga and NO upper body weights)
- 8-10 WEEKS – light weight training, yoga
DO NOT judge your breasts right away. They will not assume their final shape for at least 3 months (but they should start looking very good within 7-10 days!).
Healing is usually a very quick process though you may experience:
- Bruising around the incision and lower pole of the breast usually reaches its peak during the first week, and generally takes about 2 weeks to a month to completely fade away.
- Either a numb or a burning sensation in your nipples for about 2 weeks. This is perfectly normal and should subside as your bruising fades.
- Small patches of numbness near the incisions. These usually disappear over time, but may be permanent in some patients.
- Breast sensitivity for 2 to 3 weeks, so you might want to keep contact to a minimum.
- Mild soreness, similar to a hard workout, up to 3 to 4 weeks after surgery.
- Milk leaking from your nipples if have nursed an infant within a year of your augmentation. Should this occur, we can prescribe a medication to treat this.
To optimize and accelerate healing, we also recommend coming into the office for Bioptron and hyperbaric oxygen treatments.
MINIMIZING SCARS
Scars may likely be firm and pink for at least 6 weeks (significantly less so with incisions around the areolae). Do not worry, in a few months, they will start fading and eventually may become indetectible.
Visible scarring can be kept to a minimum by:
- Following all post-op instructions to the letter
- Where the surgical bra as recommended
- Avoiding pulling and tension
- Sleeping on your back (which keeps pressure off the implants)
- Leaving Steristrips on for 2-3 months or silicone scar strips if you develop an allergy to the former
- Avoiding all sun exposure on your neck, breasts and decolletage or at the very least using a strong physical and SPF sunblock on exposed areas
Risks and Challenges
Conditions that make augmentation mammoplasty more of a challenge and may require additional skills and surgical techniques include:
- Previous breast enhancement surgery. Surgical options may range from simply replacing the implants and removing scar tissue (capsulectomy) to complicated pocket modification (capsulorraphy) to modify how the actual implant lies under the breast. Whatever is needed, the final appearance of the breast will be rendered more natural and pleasing to both sight and touch.
- Previous breast cancer surgery and reconstruction.
- Still nursing or milky discharge. Dr Haworth delays any implant surgery for at least six months from the time lactation stops.
No surgery is entirely risk-free. However, both our staff and facilities have the highest possible qualifications and exacting standards to produce a happy outcome.
While risks and complications are generally rare, be aware that those for breast augmentation can include:
- Capsular contracture where the scar around the implant starts to shrink tight resulting in noticeable hardness and distortion of the breast. We can treat this with conservative methods or by removing the scar tissue and, in extreme cases, by replacing the implant itself. Note that while the national average for capsular contraction is 25% to 40% for implants placed above the muscle, it is less than 15% when the implant is below the muscle. Dr. Haworth’s record is far superior to this being at 6%.
- Excessive bleeding to the extent that it causes swelling and pain. Should this continue, you may need another surgery to control the bleeding and remove the accumulated blood (very rare).
- Infection around the implant, usually within a 10-14 days of the surgery. In severe cases resistant to oral medication, the doctor may need to remove the implant for several months until the infection clears and he can insert a new one (very rare).
- Change in nipple sensitivity, including numbness or over-sensitivity of the nipples
- Hematoma (blood collection within the pocket, which is also rare)
- Implant rupture, breakage or leakage
An implant rupture is uncommon but it does, and has, happened due to injury, extreme pressure or friction between the breast and implant. A saline-implant leak is harmless (saline being present in great quantities in the body) and the implant can be replaced immediately.
Dr Haworth favors the newer “Memory Gel” silicone implants produced by Mentor corporation, since they combine unparalled softness with an impressive track-record of safety and reliability. They are now FDA approved for all patients except for those under 22 years old for some questionable reason. Indeed, Dr Haworth finds it puzzling that women over 18 can legally fight in war, participate in adult films, drive while those over 21 can drink alcohol, but are considered too immature to opt for silicone breast implants! Over 90% of his patients opt for this implant choice upon weighing all the “pros and cons” and the vast majority are glad they did so. (A break in the older type of silicone implant, on the other hand, was more serious because the implant was filled with a more runny or liquid type of silicone. The thin gel tended to pool in the breast and possibly migrate to nearby lymph nodes.)
A break in either a silicone or saline-filled implant requires another surgery to exchange the implant and possibly remove scar tissue and any gel from the pocket. In some cases, it may not be possible to locate and remove all of the escaped silicone gel.
Several years ago, a number of women who had had silicone gel breast augmentation reported symptoms consistent with auto immune connective tissue disorders such as scleroderma and other arthritis-like conditions. However, numerous clinical trails conducted by the FDA concluded that there is no clear link between silicone breast implants and autoimmune disorders. The silicone implant has been the most extensively studied “device” in the whole history of medicine.
Breast implants should not affect fertility, pregnancy, or your ability to nurse.
FAQs
1. SOME OF MY FRIENDS HAVE FAKE-LOOKING BREASTS. HOW DO YOU AVOID THAT?
One must understand that many factors can contribute to the fake look. One reason is if a patient sports too large a bust line for her frame-(Think about it…How many very few slender, 0- 2 sized women naturally have DD-cup breasts?). Therefore, no matter how natural-looking the actual breast itself is, the total balance of the woman’s body will appear unnatural and top-heavy. Another reason is to have an implant above the muscle, especially in patients with little breast tissue and body fat. Ripples and, often times, the edges of the implant will become visible in these cases. The implants may appear “stuck on”. Finally, in order for the breast to fall and feel natural, the pocket in which they are placed needs to be somewhat larger than the implant itself, otherwise, the implant will not move properly and may ride up too high on the chest wall. This situation can occur if the surgeon doesn’t create an appropriate pocket or space in the first place or if the pocket shrinks down by itself. This latter situation is called encapsulation.
2. WHAT APPROACH DO YOU USE TO PUT IN THE IMPLANTS?
I almost always use the submuscular periareolar approach (or “through the nipple”) since in my hands, it affords the greatest visibility for the surgeon during surgery. As a result, I can see every millimeter of pocket creation that I perform before placing the implants within that space while enabling me to stop any bleeding that is encountered. This is in contrast to approaches through the axilla (armpit) and umbilicus (belly button-TUBA technique) which are basically “blind” procedures because the surgeon can only feel if he is creating symmetrical pockets and cannot actually visually verify the symmetry. As a result, these “blind ” procedures result in more breast implant asymmetries, “high-riding” implants, encapsulations (“hardening”) and hematomas (the latter two from uncontrolled bleeding). Patients are understandably concerned over the scarring along the areolar border with the normal breast skin as well as loss of sensation. I have found that the scarring associated with the periareolar technique of breast augmentation is almost invariably better and invisible as compared with the other approaches, including the axillary one. Loss of sensation with the periareolar incision has been found to be no different than with other methods. This is because the nerves that supply the nipple don’t run along the skin (where they can be interrupted by an incision) , but attach themselves to the nipple from its undersurface (like the roots of a tree). However, changes of nipple sensitivity are more common when larger implants are utilized.
By employing the submuscular or “below the muscle”(pectoralis major muscle) approach, one benefits from 5 ways:
- The breast tends to look better as long as the surgeon knows what they are doing by going under the muscle;
- There is less long-term sag under the muscle;
- There is less chance of seeing ripples and the edge of the implant (the latter imparting the “stuck-on” look) by going under the muscle;
- There is less interference with mammography and , finally,
- There is less chance of encapsulation (refer to 7. And 8. below).
3. WHEN DO YOU USE SILICONE IMPLANTS? WHAT ARE THE “GUMMY BEAR”/COHESIVE GEL IMPLANTS?
One must understand that there is no perfect implant which will satisfy the unique needs of every single patient. For some, saline implants are the best choice, while for others silicone may be preferable. Silicone does feel softer and more natural than saline even though it is associated with a slightly higher risk of capsular contracture (albeit by a very small amount). For the same volume, moderate profile silicone gel implants are flatter and wider while saline tends to stand taller, but with a narrower footprint. For example, a 500 cc gel implant is more like the Pentagon while a saline implant tends to be tall and narrow like a skyscraper. The choice of implant would have particular implications in patients who have a long vertical distance between their collarbones and the top of their breasts (such as after nursing). A flatter silicone implant will tend to gracefully fill this empty vertical distance lending a natural youthful appearance to the bustline without giving too much obvious forward projection, which may make a woman feel too “top-heavy”. Additionally, silicone is associated with less annoying rippling than saline.
Despite the hype about less complications associated with the solid silicone “gummy bear” implants, I have removed a number of them because of hardening/encapsulation and , even in the best of circumstances, they feel “rubbery” and more unnatural than the best regular gel implants. One must also remember that the silicone gel implants that I utilize are Mentor’s “Memory Gel” variety, which if ruptured, do not spill and yet retain their shape despite the softer consistency of the contained silicone as compared with the Cohesive Gel implants.
4. WHEN DO YOU USE TEXTURED VERSUS SMOOTH IMPLANTS? DO YOU USE THE “TEAR DROP” SHAPED IMPLANTS?
I rarely use textured implants. I find the evidence suggesting less incidence of capsular contracture associated with textured implants non-compelling, since none of the comparison studies address all other variables affecting rates of capsular contraction. For example, no study compares capsular contraction of textured implants against smooth implants implanted with the vertical submuscular megapocket technique (the one I employ) with vigorous postoperative implant- displacement massage routines. I used to use the “tear drop” implant back in 1994-1996, but have since abandoned them because the results were not consistently natural, cleavages were too far apart and the implants could rotate on themselves. My goal is to give everyone of my patients a completely natural “tear drop” shaped breast, but plastic surgeons have found that “tear drop” shaped implants tend to produce the opposite.
5. HOW DO YOU FIGURE OUT THE SIZE OF THE IMPLANTS I WILL NEED TO GET THE RESULTS I AM EXPECTING?
The most reliable to do this is to have you, the patient, collect photographs of breasts and shoulders that you like. The internet, “Playboy”, “Perfect 10” magazine, etc. are sources of these materials. I can then get a visual idea of what you desire-what is too big and conversely, what is too small. With these photos as a guide in the Operating Room, I then place “sizers” within the cavity I have created and sit you up (you are asleep of course). My nurses and I then judge how closely your breasts (with the sizers in ) match the pictures you identify with and make any adjustments as deemed necessary. After I make my determination, then I substitute the sizers for the “real” implants, again, verifying symmetry and natural hang. This protocol eliminates guesswork enabling me to best match your goals.
6. WHAT HAPPENS IF THE IMPLANT RUPTURES?
If a saline implant ruptures, one will soon notice an obvious change in the symmetry of one’s breasts (one breast will suddenly get smaller). The saline will be harmlessly absorbed by your body. On the other hand, if a gel ruptures, one may not notice any size change and indeed, the rupture may be “silent”. Only an MRI will have the best chance of non-invasively detecting if a silicone implant has ruptured. If this does occur, most of the time the gel will remain within the pocket bounded by the capsule without any health consequences. Rupture rates for Mentor gel implants have been reported to be as low as 0.5% at 3 years. I utilize Mentor implants because I prefer their texture and safety profile and all are guaranteed for life. Therefore, if one should break during the lifetime of a patient, the implant company will replace the implant free-of-charge. They will also cover the costs of surgery should an implant rupture during the first 3-5 years after the original augmentation.
7. WHAT ARE THE MAIN RISKS OF BREAST IMPLANTS?
1. 8-14% Nipple sensitivity changes (either less or more, irrespective of whether the initial incision is made around the areola or under the breast or through the umbilicus or through the axilla). Sensory changes become more prevalent when larger implants are utilized.
2. 1-2% Hematoma (a blood collection that may develop in the pocket generally within 24 hours after surgery). Should this happen, surgical drainage is all that is needed.
3. 1-2% Infection. Unfortunately, if the implant becomes infected, antibiotics will not work and removal of the implant for 3 months is indicated. This may be a psychological burden to the patient (and the surgeon), but before you know it 3 months have gone by and another implant will be in place. Fortunately, my rate of infection at The Beverly Hills Surgical Center, Inc in The Haworth Institute is only 0.5%.
4. 15-20% is the national rate of encapsulation for implants placed under the muscle while it approaches 25-50% above the muscle (depending on which study you read). My rate for under-the-muscle augmentation is roughly 10%. When I create the pocket under the muscle during surgery, I deliberately form a space that is vertically larger than the height of the implant when sitting on its end. This maneuver allows the implant to move up and down in conjunction with the patient’s overlying breast tissue in accordance to their posture. Hence, the implants will not be “affixed” in an immobile manner to the chest wall. Within a few days after surgery, the patient’s body forms a collagen-lining of the pocket that is slick to the touch. Encapsulation occurs when this pocket-lining contacts thus shrinking the pocket that I created down to the point that it is compressing and distorting the implant in a cocoon-like process. This results in an externally deformed and hardened breast. If you are unfortunate to experience an encapsulation, fortunately chances are that only one breast will be affected while the other will remain beautifully soft. This scenario indicates that something unique happened to that one affected breast pocket, otherwise both pockets would show encapsulation at the same time. The most likely event that would cause encapsulation of only one pocket would be a small amount of bleeding stemming from when a patient overexerts herself too soon after the surgery (while the tissues are fresh and still healing). That is why it is imperative to avoid all upper body exercise (including yoga and pilates and weights) for 10 weeks after breast augmentation.
8. WHAT ARE MY OPTIONS IF MY BREASTS ENCAPSULATE?
Read 7. before reading this FAQ. Conservative treatment is started early (usually more vigorous massage and Accolate™) which helps about 50% of patients. If this doesn’t completely work, then a simple operation called a Capsulectomy is performed which corrects the encapsulation for the long-term in 90% of cases. Most encapsulations occur within the first 3-4 months after the original augmentation. Therefore, as a commitment to my patients (and an acknowledgement that encapsulation is a shared risk), if anyone manifests encapsulation within the first year of surgery then my professional surgeon’s fee is waved, leaving the patient responsible the operating room and anesthesia costs. The capsulectomy is generally associated with very little pain and takes about 45 minutes to perform.
9. IS BREAST AUGMENTATION PAINFUL?
The pain from going “under the muscle” has been vastly diminished ever since I started instilling a long-acting local anesthetic (lasting about 3 days) into the pocket before waking the patient up. I have been performing this maneuver for over 10 years now with unparalleled success.
10. DO YOU DO OTHER PROCEDURES, SUCH AS A BREAST LIFT, AT THE SAME TIME AS AUGMENTATION?
Yes, but only if they are indicated and deemed safe to perform simultaneously.
11. CAN I BREAST FEED AFTER BREAST AUGMENTATION?
In the vast majority of cases, yes.
12. SHOULD I WAIT TO HAVE MY KIDS BEFORE BREAST AUGMENTATION?
If you are planning to have children in the next couple of years, than it would be prudent to wait till you are finished doing so. However, if the answer to your questions is “Yes, sometimes in the future, but I’m not sure when” or “When I get married” or “Not for at least 4-5 years”, then there would be no compelling reason to wait unless medical issues are a concern.



